This paper reports the results of an intervention with 3,471 abortion providers in India, Nepal and Nigeria. Following abortion care training, providers received in-person visits and virtual contacts by a clinical and programmatic support team for a 12-month period. The intervention also included technical assistance to and upgrades in facilities where the providers worked.
The Rohingya women and girls who have suffered sexual torture and humiliation and have now fled their homes most certainly deserve whatever care may alleviate some of their suffering. By not providing comprehensive reproductive health care, including contraception and safe abortion services, humanitarian agencies have taken a side, the side that opposes women’s human rights, the side that opposes science and common sense, the side that flies against established international agreements. Doing nothing speaks volumes.
This study aimed to support the development of a mobile phone intervention to support postmenstrual regulation family planning use in Bangladesh. It explored what family planning information women want to receive after having a menstrual regulation procedure, whether they would like to receive this information via their mobile phone, and if so, what their preferences are for the way in which it is delivered. Participatory interviews were conducted with 24 menstrual regulation clients in Dhaka and Sylhet divisions in Bangladesh.
This evaluation assesses the factors that influence contraceptive uptake among adolescents and young women seeking abortion care in health facilities. We analyzed client log book data from 921,918 abortion care cases in 4,881 health facilities in 10 countries from July 2011 through June 2015, and found that programmatic support to health systems, including provider training in contraceptive counseling and provision, was associated with women’s higher acceptance of postabortion contraception.
Numerous instances have been reported where women have been denied termination of pregnancy services for pregnancies arising out of rape, incest and sexual violence. There is also the rising issue of women and girls being forced by the police to keep the pregnancy in cases of incest or rape to preserve the infant to be used to retrieve DNA for evidence while prosecuting the perpetrator.
During last year’s national exams, media reported alarming cases of girls who sat the papers in delivery rooms or went into labour in the exam room. These statistics show the need for urgent action and awareness to enable the youth to manage their own sexual and reproductive health. Estimates from developing countries indicate that pregnancy and delivery complications, including unsafe abortions, are the second leading causes of death for girls below 20 years.
This is a fact sheet with statistical information on the sexual and reproductive health of adolescents in the Mexican state of Guerrero. It is meant to provide relevant information on sexual and reproductive health indicators to health and policy makers as well as recommendation for improving sexual and reproductive health services and access.

Esta publicación ofrece evidencia y una explicación de por qué Ipas insta a los gobiernos y formuladores de políticas a garantizar que todas las mujeres jóvenes, incluidas las sobrevivientes de violencia sexual, tengan acceso a servicios de atención integral de la salud sexual y reproductiva, incluidos los servicios de aborto seguro.
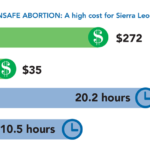
This fact sheet describes the impact of unsafe abortion in Sierra Leone as evidenced by three studies.

This is an advocacy tool for implementing authorities, service providers and NGOs on safe abortion and sex selection.

This publication highlights the work in Nepal since legal reform a decade ago and puts a spotlight on the key ingredients for successful scale-up of abortion care, including partnerships with government and NGOs and integration of abortion within the country’s Safe Motherhood program.
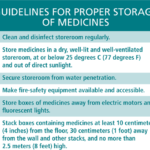

This 12-page job aid supports efficient inventory management of misoprostol (and mifepristone, depending on the setting) and other maternal-health medicines. It defines sound inventory management practices that can help reduce stock-outs and oversupply situations, and is for use by staff in public health facilities, nongovernmental organizations (civil society organizations) and private for-profit clinics and hospitals.



This is a fact sheet highlighting women’s perspectives on abortion care as part of operations research in Zambia.
Ipas works around the world every day to strengthen girls’ voices and their ability to choose the path that’s right for them.

