Last reviewed: October 12, 2022
Recommendation:
- A combination of paracervical block, nonsteroidal anti-inflammatory drugs (NSAIDs) and narcotic analgesics, with or without anxiolytics, is recommended.
- Intravenous sedation, where available, should be offered.
- The increased risks of general anesthesia must be weighed against the benefits.
Strength of recommendation: Strong
Quality of evidence: Very Low
Pain during dilatation and evacuation
A longer duration of pregnancy at the time of abortion is associated with higher reported pain scores during dilatation and evacuation (D&E) (Dzuba et al., 2022). At later gestations, D&E requires more preoperative and operative cervical dilation, longer procedure times and deeper uterine manipulation.
Methods of pain management
Comparative studies of pain management during D&E are largely lacking. Existing studies examine pain management during osmotic dilator placement before a D&E, the effect of adjuvant medications on post-procedure pain amongst people receiving general anesthesia or deep intravenous sedation, or focus instead on safety of pain management strategies during D&E. International consensus statements generally focus on the minimum amount of anesthesia at which a D&E can be performed to ensure access at lower-level facilities (Royal College of Obstetricians and Gynaecologists [RCOG], 2022; World Health Organization [WHO], 2022).
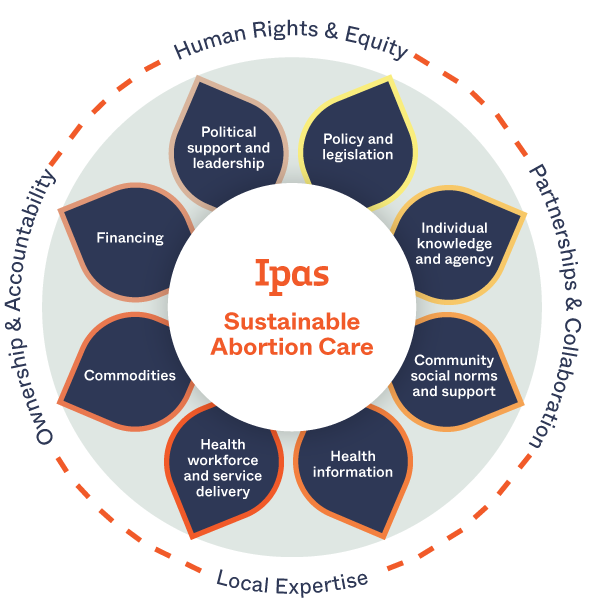
In studies reporting on D&E programs, pain management usually consists of intravenous sedation with a combination of narcotics and anxiolytics, and a paracervical block (Altman et al., 1985; Castleman et al., 2006; Jacot et al., 1993). Ipas recommends a combination of paracervical block, NSAIDs and narcotic analgesics, with or without anxiolytics (Edelman & Kapp, 2017). Where available, NSAIDs, paracervical block and intravenous sedation should be offered (Jackson & Kapp, 2020; RCOG, 2022; WHO, 2022).
Local anesthesia
See section 2.5 Paracervical block.
Medications
No studies assess the effectiveness of oral, intramuscular or intravenous pain medications during the D&E procedure. One study found that participants who received the intravenous NSAID ketorolac in combination with deep intravenous sedation or general anesthesia during their D&E procedure reported significantly lower pain post-procedure than those who did not receive the medication (Liu & Flink-Bochacki, 2021). These data must be interpreted with caution as the study was not designed to address this comparison, however, studies of vacuum aspiration have consistently found that pre-procedure administration of oral or intramuscular NSAIDs decreases pain during and after the procedure (Braaten et al., 2013; Renner et al., 2010; Romero, Turok, & Gilliam, 2008; Suprapto & Reed, 1984; Wiebe & Rawling, 1995).
Intravenous sedation
Only one randomized trial has assessed the effectiveness of intravenous moderate sedation during D&E, finding that moderate sedation with fentanyl and midazolam was significantly more effective than inhaled nitrous oxide for pain management in women between 12-16 gestational weeks who also received preprocedure ibuprofen and paracervical block (Thaxton et al., 2018). Additional data from studies of vacuum aspiration have found that intravenous sedation using a combination of narcotics and anxiolytics is an effective means of pain control and improves satisfaction with the abortion procedure (Allen et al., 2009; Allen et al., 2006; Wells, 1992; Wong et al., 2002). Studies that have assessed safety of intravenous sedation with fentanyl and midazolam in combination with paracervical block during D&E have found rates of major procedure-related complications of less than 1% (Racek, Chen, & Creinin, 2010), and no additional anesthesia-related adverse events (Gokhale et al., 2016; Wilson, Chen, & Creinin, 2009; Wiebe et al., 2013). Intravenous deep sedation with propofol and without intubation is safe and has few complications in the outpatient setting, without risk of pulmonary aspiration (Aksel et al., 2018; Dean et al., 2011; Gokhale et al., 2016; Mancuso et al., 2017).
Providing intravenous sedation increases the expense, complexity and potential risks of an abortion procedure, and it requires a trained provider with equipment for patient monitoring (Cansino et al., 2021). The increased monitoring necessary to deliver intravenous sedation safely requires facility investments in personnel, training and equipment. For further information regarding the definition of levels of sedation, including general anesthesia, see Appendix B: Continuum of depth of sedation: Definition of general anesthesia and levels of sedation/analgesia.
General anesthesia
Although effective for pain control during the procedure, general anesthesia increases the expense, complexity and potential risks associated with abortion and is not recommended for routine procedures (Atrash, Cheek, & Hogue, 1988; Bartlett et al., 2004; MacKay, Schulz, & Grimes, 1985; RCOG, 2022; WHO, 2022). For further information regarding the definition of levels of sedation, including general anesthesia, see Appendix B: Continuum of depth of sedation: Definition of general anesthesia and levels of sedation/analgesia.
Non-pharmacologic pain management
Pain medications and paracervical block should be supplemented with supportive techniques to decrease pain and anxiety. Helpful approaches may include educating the patient about what to expect during the procedure; conducting the procedure in a clean and private setting with supportive staff; providing verbal support; using gentle and efficient technique; and applying a heating pad or hot water bottle to the lower abdomen in the recovery room (Akin et al., 2001).
Resources
Continuum of depth of sedation: Definition of general anesthesia and levels of sedation/analgesis
References
Akin, M. D., Weingard, K. W., Hengehold, D. A., Goodale, M. B., Hinkle, R. T., & Smith, R. P. (2001). Continuous low-level topical heat in the treatment of dysmenorrhea. Obstetrics & Gynecology, 97, 343-349.
Aksel, S., Lang, L., Steinauer, J. E., Drey, E. A., Lederle, L., Sokoloff, A., & Carlisle, A. S. (2018). Safety of Deep Sedation Without Intubation for Second-Trimester Dilation and Evacuation. Obstetrics & Gynecology, 132(1), 171-178.
Allen, R.H., Fitzmaurice, G., Lifford, K. L., Lasic, M., & Goldberg, A. (2009). Oral compared with intravenous sedation for first-trimester surgical abortion: A randomized controlled trial. Obstetrics & Gynecology, 113(2Pt1), 276-283.
Allen, R. H., Kumar, D., Fitzmaurice, G., Lifford, K. L., & Goldberg, A. B. (2006). Pain management of first-trimester surgical abortion: Effects of selection of local anesthesia with and without lorazepam or intravenous sedation. Contraception, 74(5), 407-413.
Altman, A. M., Stubblefield, P. G., Schlam, J. F., Loberfeld, R., & Osathanondh, R. (1985). Midtrimester abortion with laminaria and vacuum evacuation on a teaching service. The Journal of Reproductive Medicine, 30(8), 601-606.
Atrash, H., Cheek, T., & Hogue, C. (1988). Legal abortion mortality and general anesthesia. American Journal of Obstetrics & Gynecology, 158(2), 420.
Bartlett, L. A., Berg, C. J., Shulman, H. B., Zane, S. B., Green, C. A., Whitehead, S., & Atrash, H. K. (2004). Risk factors for legal induced abortion-related mortality in the United States. Obstetrics & Gynecology, 103, 729-739.
Braaten, K.P., Hurwitz, S., Fortin, J., & Goldberg, A.B. (2014). Intramuscular ketorolac versus oral ibuprofen for pain relief in first-trimester surgical abortion: A randomized clinical trial. Contraception, 89(2), 116-121.
Cansino, C., Denny, C., Carlisle, A.S., & Stubblefield, P. (2021). Society of Family Planning clinical recommendations: Pain control in surgical abortion part 2-Moderate sedation, deep sedation, and general anesthesia. Contraception, 104(6), 583-592.
Castleman, L. D., Oanh, K. T. H., Hyman, A. G., Thuy, L. T., & Blumenthal, P. D. (2006). Introduction of the dilation and evacuation procedure for second-trimester abortion in Vietnam using manual vacuum aspiration and buccal misoprostol. Contraception, 74, 272-276.
Dean, G., Jacobs, A. R., Goldstein, R. C., Gevirtz, C. M., & Paul, M. E. (2011). The safety of deep sedation without intubation for abortion in the outpatient setting. Journal of Clinical Anesthesia, 23437-442.
Dzuba, I.G., Chandrasekaran, S., Fix, L., Blanchard, K., & King, E. (2022). Pain, side effects, and abortion experience among people seeking abortion care in the second trimester. Women’s Health Reports, 3.1, 533-542.
Edelman, A., & Kapp, N. (2017). Dilatation and evacuation (D&E) reference guide: Induced abortion and postabortion care at or after 13 weeks gestation. Chapel Hill, NC: Ipas.
Gokhale, P., Lappen, J. R., Waters, J. H., & Perriera, L. K. (2016). Intravenous Sedation Without Intubation and the Risk of Anesthesia Complications for Obese and Non-Obese Women Undergoing Surgical Abortion: A Retrospective Cohort Study. Anesthesia and Analgesia, 122(6), 1957-1962.
Jacot, F. R. M., Poulin, C., Bilodeau, A. P., Morin, M., Moreau, S., Gendron, F., & Mercier, D. (1993). A five-year experience with second-trimester induced abortions: No increase in complication rate as compared to the first trimester. American Journal of Obstetrics & Gynecology, 168(2), 633-637.
Jackson, E., & Kapp, N. (2020). Pain management for medical and surgical termination of pregnancy between 13 and 24 weeks of gestation: a systematic review. BJOG: An International Journal of Obstetrics & Gynaecology, 127,1348-1357.
Liu, S.M, & Flink-Bochacki, R. (2021). A single-blinded randomized controlled trial evaluating pain and opioid use after dilator placement for second-trimester abortion. Contraception, 103(3), 171-177 .
MacKay, H. T., Schulz, K. F., & Grimes, D. A. (1985). Safety of local versus general anesthesia for second-trimester dilatation and evacuation abortion. Obstetrics & Gynecology, 66, 661-665.
Mancuso, A. C., Lee, K., Zhang, R., Hoover, E. A., Stockdale, C., & Hardy-Fairbanks, A. J. (2017). Deep sedation without intubation during second trimester surgical termination in an inpatient hospital setting. Contraception, 95, 288-291.
Racek, C. M., Chen, B. A., & Creinin, M. D. (2010). Complication rates and utility of intravenous access for surgical abortion procedures from 12 to 18 weeks of gestation. Contraception, 82, 286-290.
Renner, R.M., Jensen, J.T., Nichols, M.D., & Edelman, A.B. (2010). Pain control in first-trimester surgical abortion: A systematic review of randomized controlled trials. Contraception, 81, 372-388.
Romero, I., Turok, D., & Gilliam, M. (2008). A randomized trial of tramadol versus ibuprofen as an adjunct to pain control during vacuum aspiration abortion. Contraception, 77(1), 56-59.
Royal College of Obstetricians and Gynaecologists. (2022). Best practice in abortion care. London: Royal College of Obstetricians and Gynaecologists.
Siddiqui, K. M., & Chohan, U. (2007). Tramadol versus nalbuphine in total intravenous anaesthesia for dilatation and evacuation. Journal of the Pakistani Medical Association, 57(2), 67-70.
Suprapto, K., & Reed, S. (1984). Naproxen sodium for pain relief in first-trimester abortion. American Journal of Obstetrics & Gynecology, 150(8), 1000-1001.
Thaxton, L., Pitotti, J., Espey, E., Teal, S., Sheeder, J. & Singh, R.H. (2018). Nitrous oxide compared with intravenous sedation for second-trimester abortion: a randomized controlled trial. Obstetrics & Gynecology, 132, 1182-7.
Wells, N. (1992). Reducing distress during abortion: A test of sensory information. Journal of Advanced Nursing, 17, 1050-1056.
Wiebe, E. R., Byczko, B., Kaczorowski, J., & McLane, A. L. (2013). Can we safely avoid fasting before abortions with low-dose procedural sedation? A retrospective cohort chart review of anesthesia-related complications in 47,748 abortions. Contraception, 87, 51-54.
Wiebe, E. R., & Rawling, M. (1995). Pain control in abortion. International Journal of Gynecology & Obstetrics, 50(1), 41-46.
Wilson, L. C., Chen, B. A., & Creinin, M. D. (2009). Low-dose fentanyl and midazolam in outpatient surgical abortion up to 18 weeks of gestation. Contraception, 79, 122-128.
Wong, C. Y., Ng, E. H., Ngai, S. W., & Ho, P. C. (2002). A randomized, double blind, placebo-controlled study to investigate the use of conscious sedation in conjunction with paracervical block for reducing pain in termination of first trimester pregnancy by suction evacuation. Human Reproduction, 17(5), 1222-1225.
World Health Organization. (2022). Abortion care guideline. Geneva: World Health Organization.